MINIMALLY-INVASIVE SURGERY
Colorectal Surgeons Sydney perform a variety of Minimally-Invasive Procedures, including:
ENDOSCOPIC SURGERY
Endoscopic Surgery is surgery performed through a colonoscope typically with a wire snare and diathermy and is used for many colorectal conditions.
However, its main use is for large (>1cm) benign polyps of the colon that cannot be removed with conventional snare polypectomy. It should not be used for biopsy proven polyps containing cancer, or polyps with suspicious features for having cancer in them.
The two common methods include Endoscopic Mucosal Resection (EMR) and Endoscopic Submucosal Dissection (ESD).
The advantages of endoscopic surgery, is the avoidance of an incision. The disadvantage is the risk of colonoscopic perforation which has a risk of 5% [1]. The other disadvantage of endoscopic techniques is that they are not suitable for cancers, which require a proper resection to remove not only the cancer, but the lymph nodes around the colon.
Endoscopic mucosal resection
Endoscopic mucosal resection (EMR) involves:
- the injection of a solution into the submucosal layer of the bowel wall; and
- En bloc or piecemeal resection of the lesion using a snare.
Injection fluid has traditionally been normal saline, however more recently better results have been achieved with a mixture of succinylated gelatin (Gelofusin®) with a blue colour dye (methylene blue) and adrenaline to cause vasoconstriction [2].

By injection underneath the large polyp, it allows the polyp to be lifted up off of the underlying colon wall, thus allowing more easy inclusion of the lesion in a large snare, which reducing the risk of thermal injury and perforation to the underlying colon. The main disadvantage of this technique is that piecemeal removal of the polyp is often required for very large polyps, leading to potential error when assessing the specimen for underlying cancer.
Endoscopic submucosal dissection (ESD)
Endoscopic Submucosal Dissection (ESD) can be used for larger polyps, and also involves lifting the polyp with injected solutes. The benefits of ESD include the complete en bloc removal of the specimen rather than by piece-meal [3-4].

Robotic transanal endoscopic submucosal dissection (ESD)
Robotic Transanal Endoscopic Submucosal Dissection (RTESD) was first performed in Australia in 2015 using a Gelpoint TAMIS® port and the da Vinci® SI robot[5]. The da Vinci® robot has certain advantages over previously used techniques for ESD and EMR. This is largely due to the ability of the robot’s small miniaturised robotic hands to perform complex movements including suturing within the very narrow confines of the rectum.
References
- Rembacken BJ. Fujii T. Cairns A. Dixon MF. Yoshida S. Chalmers DM. Axon AT Flat and depressed colonic neoplasms: a prospective study of 1000 colonoscopies in the UK. Lancet. 355(9211):1211-4, 2000 Apr 8.
- Moss A. Bourke MJ. Kwan V. Tran K. Godfrey C. McKay G. Hopper AD. Succinylated gelatin substantially increases en bloc resection size in colonic EMR: a randomized, blinded trial in a porcine model. Gastrointestinal Endoscopy. 71(3):589-95, 2010 Mar.
- Moss A. Bourke MJ. Tran K. Godfrey C. McKay G. Chandra AP. Sharma S. Lesion isolation by circumferential submucosal incision prior to endoscopic mucosal resection (CSI-EMR) substantially improves en bloc resection rates for 40-mm colonic lesions. Endoscopy. 42(5):400-4, 2010 May.
- Moss A, Bourke MJ, Metz AJ, McLeod D, Tran K, Godfrey C, McKay G, Chandra AP, Pasupathy A. Beyond the snare: technically accessible large en bloc colonic resection in the West: an animal study. Dig Endosc. 24 (1):21-9, 2012 Jan.
- Lajevardi SS, Tameev Z, McKay G. Robotic Transanal Endoscopic Submucosal Dissection (RTESD) of Large Rectal Tumor in Prone Position. J Minim Invasive Surg Sci. 2016 May; In Press(In Press):e34095.
LAPAROSCOPIC BOWEL SURGERY
Key-Hole (Laparoscopic) surgery has the benefit of reduced size of incision, leading to better cosmesis and reduced pain. This allows for earlier mobilisation with less, pain, and earlier resumption of normal activities including earlier return to work.
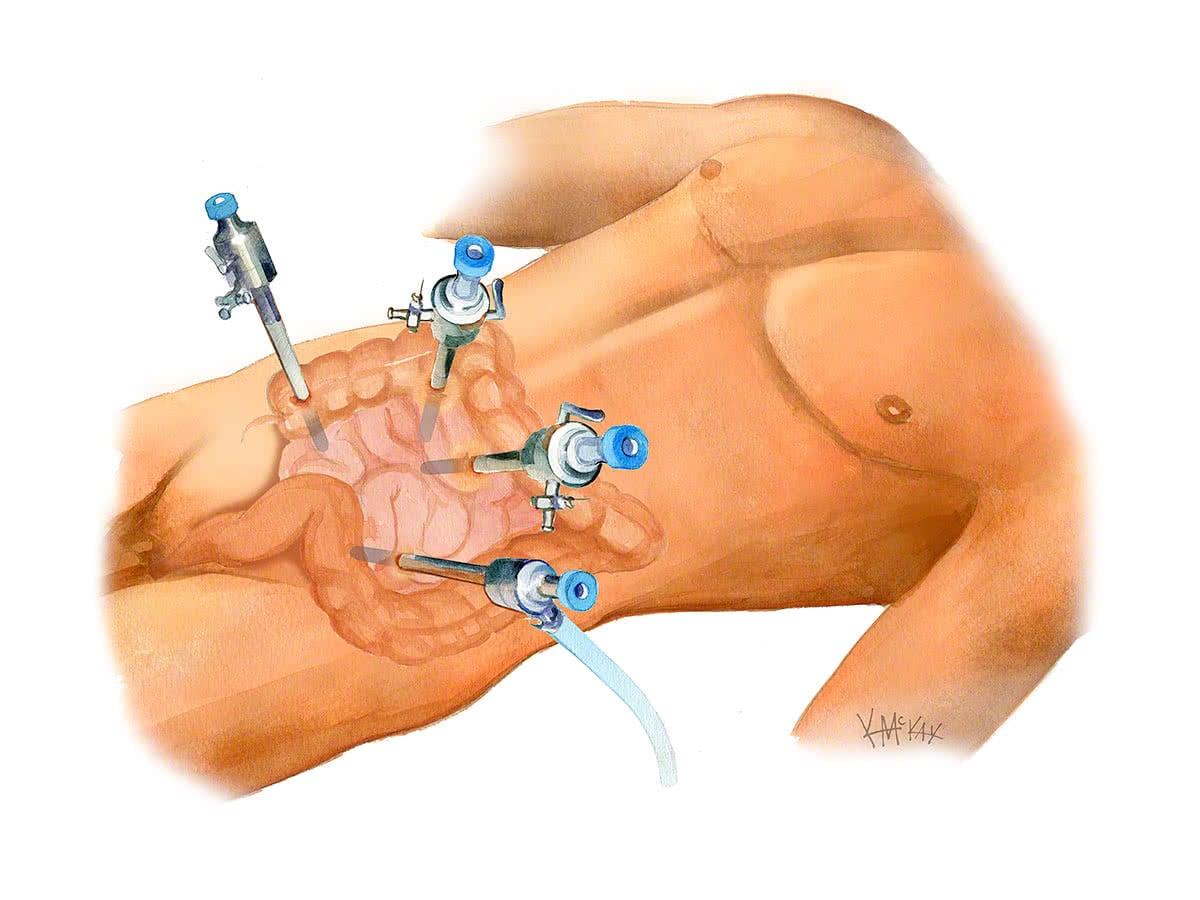
Key hole (laparoscopic) surgery has now been shown in multiple randomised controlled trials to be safe for colon cancer surgery. A large number of randomised controlled trials [1-8] and a large review[9], have shown similar benefits for rectal cancer surgery. Two large Australian studies have shown its safety for colorectal cancer with benefits in both young and elderly patients [10-11].
Robotic surgery is an emerging technology that combines the benefits of minimally invasive surgery with the fine-motor precision afforded only by robotics. It’s most useful application is for surgery low in the pelvis, making it particularly suitable for low rectal cancer surgery. It provides many of the benefits of laparoscopic surgery, with its improved control allowing for better resection margins and less blood loss.
References
- Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet 2005;365:1718-1726.
- Araujo SE, da Silva eSousa AH Jr, dr Campos FG, et al. Conventional approach laparoscopic abdominoperineal resection for rectal cancer treatment after neoadjuvant chemoradiation: results of a prospective randomized trial. Rev Hosp Clin Fac Med Sau Paulo. 2003;58:133-40.
- Ng SS, Leung KL, Lee JF, et al. Laparoscopic-assisted versus open abdominoperineal resection for low rectal cancer: a prospective randomized trial. Ann Surg Oncol 2008;15:2418-2425.
- Leung KL, Kwok SP, Lam SC, et al. Laparoscopic resection of rectosigmoid carcinoma: prospective randomised trial. Lancet 2004;363:1187-1192.
- Kang S et al. Open versus laparoscopic surgery for mid or low rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): short-term outcomes of an open-label randomised controlled trial. Lancet Oncol 2010;11:637-645.
- Zhou Z, Hu M, Li Y, et al. Laparoscopic vs open total mesorectal excision with anal sphincter preservation for low rectal cancer. Surg Endosc 2004;18:1211-1215.
- Braga M, Frasson M, Vignali A, et al. Laparoscopic resection in rectal cancer patients: outcome and cost-benefit analysis. Dis Colon Rectum 2007;50:464-471.
- Lujan J, Valero G, Hernandez Q, et al. Randomized clinical trial comparing laparoscopic and open surgery in patients with rectal cancer. Br J Surg 2009;96:982-989.
- Breukink S, Pierie J-P, Wiggers T. Laparoscopic versus open total mesorectal excision for rectal cancer. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No.: CD005200. DOI: 10.1002/14651858.CD005200.pub2.
- Allardyce RA, Bagshaw PF, Frampton CM, et al. The Australasian laparaoscopic colon cancer study. ANZ J Surg. 2008;78:832–833.
- >McKay GD, Morgan MJ, Wong SKC, et al. Improved Short-term Outcomes of Laparoscopic versus Open Resection for Colon and Rectal Cancer in an Area Health Service: A Multicentre Study. Diseases of the Colon & Rectum 2012: 55(1); page 42-50.
ROBOTIC BOWEL SURGERY
Robotic colorectal surgery with the Da Vinci® robot, allows for the benefits of minimally invasive surgery, along with the fine precision, 3D vision and magnified view afforded only by robotic surgery.
Its main advantage over open surgery is the avoidance of large incisions. The improved visibility and dexterity of robotic surgery allow for less blood loss, shorter hospital stay and faster recovery compared with open surgery.

Its main application is for difficult surgery low in the pelvis, making it particularly suitable for low rectal surgery including that for rectal prolapse and rectal cancer. Robotic surgery has been shown now to take slightly longer than conventional laparoscopic surgery [1] but results in improved resection margins and less blood loss. With improved resection margins, the risk of inadvertent nerve injury and sexual dysfunction is thought to be less.
How does robotic surgery work?
Though often called “robotic surgery”, the surgery is entirely performed by your colorectal surgeon, with miniature robotic arms inserted through just a few tiny openings. The da Vinci system has been used successfully worldwide in hundreds of thousands of procedures to date.


Transanal Surgery using the robot?
Transanal surgery using the robot was first performed in Australia in 2015 by Sydney colorectal surgeon Dr Gary McKay [2]. The robot has certain advantages over previously used techniques for removing tumours or large polyps from the rectum via the anus. This is largely due to the ability of the robot’s small miniaturised robotic hands to perform complex movements including suturing within the very narrow confines of the rectum. The benefit of such surgery is the avoidance of major abdominal surgery and preservation of the rectum and bowel continuity.
Where is robotic surgery available?
Robotic surgery with the latest XI model is available at Mater Private Hospital, Westmead private Hospital and St George Private Hospital. .
What is the added cost of robotic surgery?
Robotic surgery is not yet fully reimbursed by all health funds or Medicare, therefore there may be some additional costs that you will need to discuss with your colorectal surgeon.
What to expect pre and post operatively for robotic colorectal surgery
You will need to have only clear fluids the day before your surgery. Clear liquids are those that one can see through. When a clear liquid is in a container such as a bowl or glass, the container is visible through the substance. You will also require bowel prep to clean your colon. Take a Pico-sulfate (Picoprep®) prep at 2pm 4pm and 6pm the day before your procedure. You need to fast from midnight the night before if your surgery is scheduled for the morning, or from 6am if scheduled for the afternoon. Immediately after your procedure you will be commenced on free fluids (semi thickened fluids such as custard, yoghurt, thin porridge). The small incisions of robotic surgery allow you to mobilise from day one. You will be commenced on a light diet once you have passed flatus. You will be discharged from hospital once you have opened your bowels. A typical admission is anywhere from 3 days to 7 days.
Post operatively, you will need to see your colorectal surgeon at 3-6 weeks post-operatively to check on your progress. If your surgery is for cancer, you will then be followed up regularly (every 1-3 years), with colonoscopy performed at regular intervals.
References
- Maeso S, Reza M, Mayol JA, Blasco JA, Guerra M, Andradas E, Plana MN. Efficacy of the Da Vinci surgical system in abdominal surgery compared with that of laparoscopy: a systematic review and meta-analysis.Ann Surg. 2010 Aug;252(2):254-62.
- Lajevardi SS, Tameev Z, McKay G. Robotic Transanal Endoscopic Submucosal Dissection (RTESD) of Large Rectal Tumor in Prone Position. J Minim Invasive Surg Sci. 2016 May; In Press(In Press):e34095.
TRANSANAL ENDOSCOPIC MICRO-SURGERY (TEMS)
Transanal Endoscopic Micro-Surgery (TEMS) allows for the removal of benign polyps of the rectum without need for conventional surgery. It has many benefits over conventional surgery, is safe, and allows for early discharge being performed as a day-stay procedure. Recovery is quicker than conventional surgery with discharge from hospital the following day.
Indication for TEMS
TEMs is indicated for benign polyps of the rectum. In certain circumstances, it may have a role for early cancer within a polyp provided strict criteria are adhered to and include the following:
- Small cancer
- Cancer is not poorly differentiated
- There is no lymphovascular invasion
- Margins are clear
Salvage surgery
Patients who undergo TEMS and subsequently are discovered to not meet the above criteria should then be advised to undergo conventional surgery, with excellent survival with rates with immediate salvage surgery compared to delayed salvage surgery once a recurrence is found [1-3].
Benefits of TEMS
The benefit of TEMS over other endoscopic surgical technique (EMR AND ESD) include better exposure and control, with complete removal of the lesion in one piece. It also avoids major surgery and the need for a stoma.
What to expect pre and post operatively for TEMS surgery
A normal diet without bowel prep is required the day before surgery. You need to fast from midnight the night before if your surgery is scheduled for the morning, or from 6am if scheduled for the afternoon. You will be admitted as a day-stay procedure. You will receive a fleet® enema 1-2 hours prior to your TEMS operation.
Following your procedure, you will recover for a hour until the effects of sedatives have worn off. You should not drive yourself home after your procedure and should have someone organised (a friend or relative) to accompany you.
You will be sent home on a course of the oral antibiotic metronidazole (Flagyl®). This will prevent infection and inflammation to the surgical site. You should also remain on regular laxatives and simple analgesics for 1 week. We recommend taking twice daily a tablespoon of natural psyllium husk (Metamucil® or Fibogel®), and 30ml of lactulose (Duphalac®). It is not unusual for there to be some pain to the anal region in the first week following surgery. For pain we recommend after each meal 400mg of ibuprofen (Brufen®) and 1g of paracetamol. Opioid medications (Codeine and Morphine) should be avoided as they cause constipation.
Twice daily warm to hot salt water (sitz) bathing to the anal region is soothing and antiseptic, and should be done for 1 week following your procedure.
You should follow up with your colorectal surgeon in 6 weeks to review your wound and discuss further management if indicated.
References
- Baron PL, Enker WE, Zakowski MF, Urmacher C. Immediate vs. Salvage Resection After Local Treatment for Early Rectal Cancer. Diseases of the Colon and Rectum 38(2): 177-181, 1995.
- Friel CM, Cromwell JW, Marra C, et al. Salvage radical surgery after failed local excision for early rectal cancer. Dis Colon Rectum. 2002;45:875– 879.
- Hahnloser D, Wolff B, Larson D, Ping J, Nivatvongs S. Immediate radical resection after local excision of rectal cancer: an oncologic compromise? Diseases of the Colonand Rectum 48(3): 429-37, 2005.